(5-10 minute read)
Shoulder injuries are a significant concern for athletes in overhead sports like tennis, handball, and volleyball. The incidence of these injuries range from 18% to 61%, depending on factors such as sports type, gender, and age9. For physiotherapists and sports clinicians, determining an athlete’s readiness to RTS while minimising the risk of re-injury is crucial.

How can a clinician be confident at getting athletes safely back to sports following shoulder injury?
In this blog I will cover the 5 outcome measures clinicians should assess when determining an athlete’s readiness to return to overhead sports:
- Shoulder Strength
- Range of Motion
- Pain
- Functional Patient-Reported Outcome Measure
- Psychological Patient-Reported Outcome Measure
Below is an infographic with a summary of this blog:
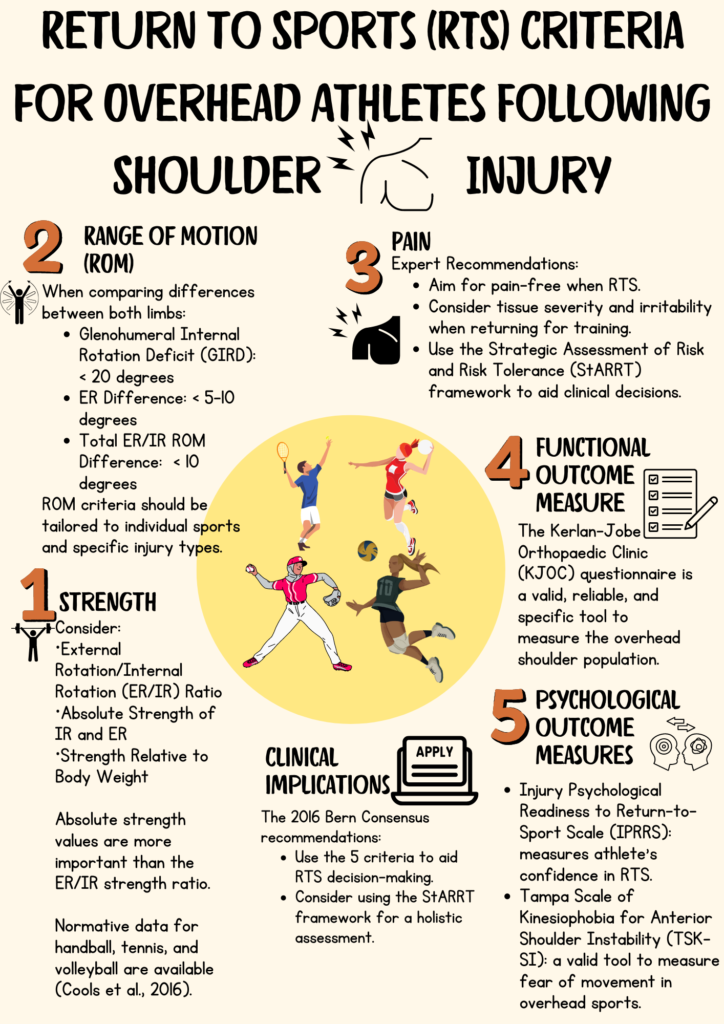
RTS Criteria for Overhead Athletes After A Shoulder Injury
Current research on RTS criteria for shoulder injuries is somewhat limited3, 9, emphasising the need for evidence-based practice supported by clinical expertise and guidelines8. The 2022 Bern Consensus outlines five key outcome measures for RTS criteria9:
1) Shoulder Strength
Considerations: Strength assessment should focus on:
- External Rotation/Internal Rotation (ER/IR) Ratio
- Absolute Strength of IR and ER
- Strength Relative to Body Weight
The literature provides normative data for the ER/IR ratio and absolute strength for handball, tennis, and volleyball4. Clinicians are encouraged to search for normative data specific to their athletes’ sports.
When comparing athletes’ strength within a team, the clinician should normalise their body weight for accurate comparison4, 9.
Implications:
Absolute strength values are more important than the ER/IR strength ratio9. Clinicians must consider the absolute values when testing for strength. An athlete might score well on the ER/IR strength ratio but still have low overall muscle strength, increasing their risk of injury 3.
2) Range of Motion (ROM)
Clinical tips: Overhead sports athletes tends to develop an increased in glenohumeral ER and decrease in glenohumeral IR in the dominant arm. This changes appears to be an adaptive response to the demands of their sports. The exact causes of this change are uncertain, but they may be caused by bony adaptation, posterior capsule tightness, muscular weakness and tightness, or a combination of all these factors13,14.
So be mindul of this adaptation when measuring your athletes ROM.
Controversy: Evidence on Glenohumeral Internal Rotation Deficit (GIRD) as a predictor of injury is mixed6. A systematic review of 2,195 athletes found no significant link between ROM deficits and injury risk, though this study had limitations such as poor methodological quality and limited generalisability to baseball players6.
In another study comparing the shoulder mobility of 47 professional World Tour tennis players with and without a history of pain found no significant side-to-side asymmetries in ROM. However, the pain history group exhibited significantly less internal rotation in both shoulders and a reduced total arc of motion compared to the non-pain history group. In summary, athletes with a history of shoulder pain tend to have decreased internal rotation and total rotational ROM. Therefore, it is crucial to compare these athletes against a healthy population, especially when addressing bilateral shoulder pain12.
Although there are conflicting results on whether GIRD or reduced total rotational ROM do increase the risk of injuries, experts recommend the following when comparing between sides3:
- GIRD: < 20o
- External Rotation Difference: < 5-10o
- Total ER/IR ROM Difference: < 10o
Implications:
ROM criteria should be tailored to individual sports and specific injury types9. Restoring pre-injury ROM may not always be feasible, particularly after surgeries like shoulder stabilisation. Comparing results with normative data when it is available is useful especially if the athlete has bilateral shoulder pain history.
3) Pain
Expert Recommendations:
- Athletes may return to training with some pain, but they should be pain-free when performing at their pre-injury level9.
- Clinicians should assess tissue irritability and severity by analysing pain during activity, after activity, and at night to guide the RTS process3.
- The Strategic Assessment of Risk and Risk Tolerance (StARRT) framework can be helpful in this decision-making process, involving athletes, coaches, and medical staff collaboratively3, 9, 10.
4) Functional Patient-Reported Outcome Measures (PROMs)
Kerlan-Jobe Orthopaedic Clinic (KJOC) Questionnaire: This tool is recommended over the Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire for assessing functional outcomes in overhead shoulder athletes. The KJOC is more valid, reliable, and responsive for this population1.
Clinical tips: Check out the KJOC questionnaire and compare that with other PROMs you use. Which content do you think are more specific for the overhead sporting population?
5) Psychological PROMs
It is important to assess the psychological readiness and kinesiophobia when making RTS decisions5,7, 11. Fear of movement can lead to poor movement patterns, worsening shoulder pain, impaired physical function, and a lower quality of life7, 11. Neglecting the psychological aspects may put athletes at risk of re-injury5, 9.
- Injury Psychological Readiness to Return-to-Sport Scale (IPRRS): This is a valid tool in assessing psychological readiness in RTS for non-professional athletes suffering from various musculoskeletal injuries5.
- Tampa Scale of Kinesiophobia for Anterior Shoulder Instability (TSK-SI): This is a modified tool from the original TSK to assist clinicians in assessing and evaluating the severity of fear of movement, specifically in patients experiencing anterior shoulder instability11. It has been tested for content validity to determine kinesiophobia in the shoulder population and can be useful for overhead shoulder athletes. Further research is needed to assess its external validity on larger groups and overhead athletes.
Implications: Psychological readiness is crucial for athletes returning to sports. Athletes should feel comfortable and have low fear of reinjury before advancing to the next phase of their RTS process9.
Limitations of Current Research
Current research often lacks methodological rigor and is not always applicable across different sports. There is a need for studies that examine the interplay between extrinsic and intrinsic factors, including sport-specific risks. Future research should adopt a biopsychosocial approach, integrating injury-specific and individual factors to better inform RTS decisions2.
Conclusion
A comprehensive approach to RTS criteria involves evaluating strength, ROM, pain, functional and psychological aspects. Despite the current limitations in research, using a combination of these measures and tools like the StARRT framework can guide clinicians in making informed RTS decisions. Future research should focus on filling gaps in knowledge and improving methodological approaches to enhance our understanding of effective RTS strategies.
References:
- Alberta, F. G., ElAttrache, N. S., Bissell, S., Mohr, K., Browdy, J., Yocum, L., & Jobe, F. (2010). The development and validation of a functional assessment tool for the upper extremity in the overhead athlete. The American Journal of Sports Medicine, 38(5), 903–911. https://doi.org/10.1177/0363546509355642
- Bittencourt, N. F. N., Meeuwisse, W. H., Mendonça, L. D., Nettel-Aguirre, A., Ocarino, J. M., & Fonseca, S. T. (2016). Complex systems approach for sports injuries: Moving from risk factor identification to injury pattern recognition—narrative review and new concept. British Journal of Sports Medicine, 50(21), 1309–1314. https://doi.org/10.1136/bjsports-2015-095850
- Cools, A. M. J., Maenhout, A. G., Vanderstukken, F., Declève, P., Johansson, F. R., & Borms, D. (2021). The challenge of the sporting shoulder: From injury prevention through sport-specific rehabilitation toward return to play. Annals of Physical and Rehabilitation Medicine, 64(4), 101384–101384. https://doi.org/10.1016/j.rehab.2020.03.009
- Cools, A. M. J., Vanderstukken, F., Vereecken, F., Duprez, M., Heyman, K., Goethals, N., & Johansson, F. (2016). Eccentric and isometric shoulder rotator cuff strength testing using a hand-held dynamometer: Reference values for overhead athletes. Knee Surgery, Sports Traumatology, Arthroscopy : Official Journal of the ESSKA, 24(12), 3838–3847. https://doi.org/10.1007/s00167-015-3755-9
- Dluzniewski, A., Casanova, M. P., Ullrich-French, S., Brush, C. J., Larkins, L. W., & Baker, R. T. (2024). Psychological readiness for injury recovery: Evaluating psychometric properties of the IPRRS and assessing group differences in injured physically active individuals. BMJ Open Sport & Exercise Medicine, 10(2), e001869. https://doi.org/10.1136/bmjsem-2023-001869
- Keller, R. A., De Giacomo, A. F., Neumann, J. A., Limpisvasti, O., & Tibone, J. E. (2018). Glenohumeral internal rotation deficit and risk of upper extremity injury in overhead athletes: A meta-analysis and systematic review. Sports Health, 10(2), 125–132. https://doi.org/10.1177/1941738118756577
- Kim, M., Haratian, A., Fathi, A., Kim, D. R., Patel, N., Bolia, I. K., Hasan, L. K., Petrigliano, F. A., & Weber, A. E. (2023). Can we identify why athletes fail to return to sports after arthroscopic Bankart repair? A systematic review and meta-analysis. The American Journal of Sports Medicine, 51(9), 2480–2486. https://doi.org/10.1177/03635465221089980
- Sackett, D. L., Rosenberg, W. M. C., Gray, J. A. M., Haynes, R. B., & Richardson, W. S. (1996). Evidence based medicine: What it is and what it isn’t: It’s about integrating individual clinical expertise and the best external evidence. BMJ (Online), 312(7023), 71–72. https://doi.org/10.1136/bmj.312.7023.71
- Schwank, A., Blazey, P., Asker, M., Møller, M., Hägglund, M., Gard, S., Skazalski, C., Haugsbø Andersson, S., Horsley, I., Whiteley, R., Cools, A. M., Bizzini, M., & Ardern, C. L. (2022). 2022 Bern Consensus Statement on shoulder injury prevention, rehabilitation, and return to sport for athletes at all participation levels. The Journal of Orthopaedic and Sports Physical Therapy, 52(1), 11–28. https://doi.org/10.2519/jospt.2022.10952
- Shrier, I. (2015). Strategic Assessment of Risk and Risk Tolerance (StARRT) framework for return-to-play decision-making. British Journal of Sports Medicine, 49(20), 1311–1315. https://doi.org/10.1136/bjsports-2014-094569
- van Iersel, T. P., Larsen van Gastel, M., Versantvoort, A., Hekman, K. M. C., Sierevelt, I. N., Broekman, B. F. P., van den Bekerom, M. P. J., den Arend, M. C., Boon, F., Versluis, E. J., van Noort, A. V. N., Alta, T. D., Portegies, S., Haas, I. S., Schmitz, P. M., de Fockert, L. H., Raven, E. E. J., Tijhaar, L. M., Nordkamp, R. A. G., … Engelsma, Y. (2023). The modified Tampa-scale of kinesiophobia for anterior shoulder instability. Arthroscopy, Sports Medicine, and Rehabilitation, 5(4), 100768–100768. https://doi.org/10.1016/j.asmr.2023.100768
- Moreno-Pérez, V., Moreside, J., Barbado, D., & Vera-Garcia, F. J. (2015). Comparison of shoulder rotation range of motion in professional tennis players with and without history of shoulder pain. Manual Therapy, 20(2), 313–318. https://doi.org/10.1016/j.math.2014.10.008
- Crockett, H. C., Gross, L. B., Wilk, K. E., Schwartz, M. L., Reed, J., OMara, J., Reilly, M. T., Dugas, J. R., Meister, K., Lyman, S., & Andrews, J. R. (2002). Osseous adaptation and range of motion at the glenohumeral joint in professional baseball pitchers. The American Journal of Sports Medicine, 30(1), 20–26. https://doi.org/10.1177/03635465020300011701
- Reagan, K. M., Meister, K., Horodyski, M. B., Werner, D. W., Carruthers, C., & Wilk, K. (2002). Humeral retroversion and its relationship to glenohumeral rotation in the shoulder of college baseball players. The American Journal of Sports Medicine, 30(3), 354–360. https://doi.org/10.1177/03635465020300030901
